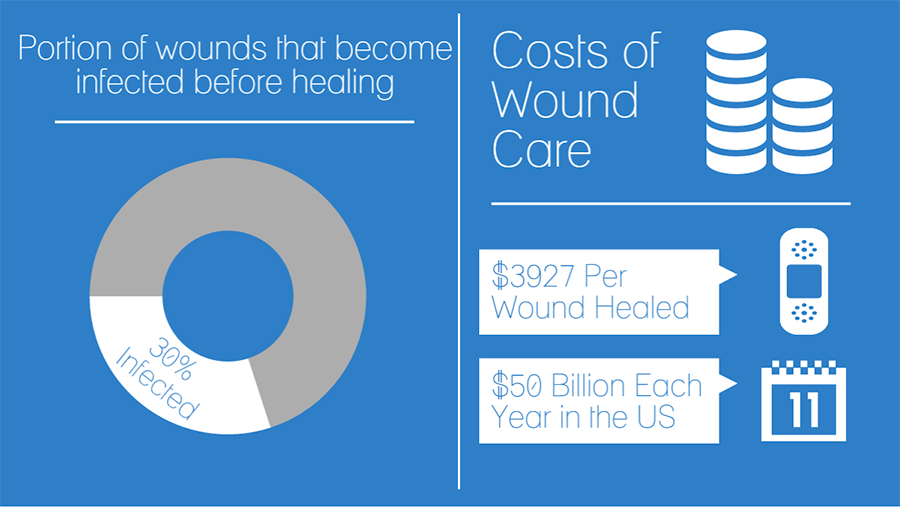
Wounds are a significant problem for hospitals, hospices, and other treatment facilities. Over 35% of hospice patients are affected by wounds, with many more in hospitals and clinics.1 For all of these patients, dressings must be changed regularly and wounds must be frequently cleaned. This means that wound care makes up a large portion of nurses’ duties and costs health care facilities a significant amount of money, with the mean cost to heal per wound an estimated $3927, according to one recent study. 2
The high financial and time costs of wound care are compounded by the fact that wound dressings are prone to peeling at the sides. This causes them to fall off more easily, and increases the likelihood that foreign substances, such as fecal matter and urine, can enter the wound. This may increase the chance of infection in the wound and could lead to prolonged wound treatment and worse outcomes for patients. 3, 4
A more secure wound dressing
Given the prevalence of wounds and the amount of time wound care requires from nurses, it is beneficial to ensure that wound dressings are as secure and long lasting as possible. This can reduce the frequency with which they need to be changed and reduce the risk that the wound will become infected. A secure wound dressing should stay firmly attached to the affected area, without any peeling.
Many otherwise effective dressings are compromised by their ability to stay attached to the wound area. A more effective means of securing the dressing could make these products longer lasting and better able to block out possibly infectious material.
The Value of More Secure Dressings
A more secure dressing could provide several benefits to nurses, patients, and health care facilities, including reduced costs, less time spent changing dressings, and improved outcomes for patients.
Secure dressings are more effective
One of the primary goals of wound care is to decrease the risk that the wound becomes infected. However, despite these intentions, as many as 30% of wounds become infected at some point before healing. 3 This can lead to an increase in the time it takes for the wound to fully heal and result in other potentially dangerous complications.4
Peeling at the corners could increase the likelihood of an infection, particularly in cases where the patient suffers from incontinence. If a dressing does not fully cover the wound, it may be exposed to foreign substances. Fecal matter and urine can introduce bacteria into the wound that can lead to infection or other complications. Prolonged exposure to feces can also cause incontinence associated dermatitis, further damaging the skin, particularly in older populations.5
Another major problem in wound care is ensuring compliance in outpatients. When a patient goes home, they may be more active and the dressing may be exposed to non-ideal conditions. More secure dressings could increase the length of time dressings remain on outpatients in trying conditions, further increasing their effectiveness.
Secure dressings reduce wasted time and money
Treatment of chronic non-healing wounds in the United States costs an estimated $50 billion each year. Wound incidence is increasing at a rate of 10% each year, so these costs are only expected to grow. 2, 6 The two major contributing factors to this expenses are the costs of the dressings themselves and the man hours nurses must spend on wound care.
Nurses spend a considerable amount of time cleaning, dressing, and caring for wounds. One recent study found that a community of 288,000 with a wound prevalence of 2.4 per 1000 residents requires the equivalent of 57 full-time nurses for dressing changes alone. 7 More secure dressings that required fewer changes could significantly reduce the time nurses must spend on wound care, allowing them to focus on other patient concerns and helping to reduce costs. The wound dressings themselves can also be a considerable expense, and can cost from $10 to $20 daily per dressing, or even more depending on the type of dressing and size of wound. 8 Over time, this expense can amount to a considerable sum, significantly impacting the facility’s finances and adding to the overall cost of treatment. A dressing that stayed secure and did not need to be replaced as often could help reduce the number of dressings that needed to be purchased.
How Hy-Tape Can Help with Secure Dressings
Hy-Tape is the leading surgical adhesive, helping to make wound dressings more secure, more effective, and less costly. By framing or covering dressings with Hy-Tape, nurses can reduce the risk of peeling corners and know their dressings will stay on longer.
Hy-Tape makes dressings more secure – Hy-tape is very secure and lasts up to seven days. That means that it can help dressings stay on for longer. It is also waterproof, so it is not affected by drainage fluids, urine, feces, or other liquids that might normally compromise the integrity of the dressing.
Hy-Tape protects the wound – Hy-tape does not break down and does not allow fecal matter and urine to infect the wound. It is also completely washable, allowing foreign substances to be cleared away without damaging the dressing. This could help reduce the risk of infection and may even help wounds heal faster in certain conditions.
Hy-tape is gentle – Despite its ability to stay secure even in the most trying circumstances, Hy-Tape is gentle and easily removed. It will never cause new wounds or further damage the existing wound. Its zinc-oxide based adhesive is soothing to delicate skin and prevents irritation and skin breakdown.
Hy-tape is nurse approved – In a recent study involving patients with Stage II, III, and III pressure sores treated with a hydrocolloid dressing secured by Hy-Tape, Hy-tape was given an “Excellent” rating by nurses. They cited its strength, gentleness, and easy application as primary reasons for the high rating. 9
To learn more about how Hy-Tape can help make wound dressings longer lasting and more effective, contact one of our representatives today.
REFERENCES:
[1] Reifsnyder J, Hoplamazian L. Incidence and Prevalence of Pressure Ulcers in Hospice Setting.
[2] Fife, E. Caroline; Carter, Mellissa; Walker, David; Thomson, Brett. Wound Care Outcomes and Associated Cost Among Patients Treated in US Outpatient Wound Centers: Data From the US Wound Registry.WOUNDS 2012;24(1):10-17. http://www.woundsresearch.com/article/wound-care-outcomes-and-associated-costamong-patients-treated-us-outpatient-wound-centers-d
[3] Lindholm C. Pressure Ulcers and Infection—Understanding Clinical Features. Ostomy Wound Management. Vol. 49, Issue 5A, May 2003. pp. 4-7.
[4] Guo, S. Factors Affecting Wound Healing. J Dent Res. 2010 Mar; 89(3):219–229. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2903966/
[5]Faecal Incontinence and Its Effect on Wound Care. Continence Essential. Volume 1 2008. http://www.continence-uk.co.uk/essentials_2008/Continence_Essentials_2008_Faecal_Incontinence_Wound_Care.pdf
[6] Cuddigan J, Berlowitz D, Ayello E. Pressure Ulcers in America: Prevalence, Incidence, and Implications for the Future: An Executive Summary of the National Pressure Ulcer Advisory Panel Monograph. Advances in Skin & Wound Care: The Journal for Prevention and Healing. July/August 2001; Volume 14 Number 4: pp. 208-215.
[7] Lindholm, C., Bergsten, A., Berglund, E. Chronic wounds and nursing care. Journal of Wound Care 1999; 8: 1, 5-10.
[8] Comparison of homecare costs of local wound care in surgical patients randomized between occlusive and gauze dressings.Ubbink DT1, Vermeulen H, van Hattem J. J Clin Nurs. 2008 Mar;17(5):593-601. doi: 10.1111/j.1365-2702.2007.02032.x.
[9] Securing Hydrocolloid Dressing. Hy-Tape. http://www.hytape.com/pdfs/HTCase-Studies-Ostomy-Wound%20Care2.pdf. Accessed May 2015.