Secondary dressings can be an effective tool to protect the primary dressing or provide additional functionality beyond the primary dressing. Hydrocolloid or foam dressings can provide protection for the wound area and manage excess exudate. However, they can also significantly add to the cost and time of wound care. This makes it critical that health care professionals implement effective practices to extend wear time of secondary dressings.
Challenges of Extending Secondary Dressing Wear Time
Secondary dressings may need to be removed or replaced for a wide range of reasons, depending on their intended purpose, type, and how they are placed. Understanding these challenges and taking steps to preempt them can greatly extend secondary dressing wear time.
Movement of Primary Dressing – The secondary dressing must hold the primary dressing in its intended place. If the underlying dressing moves, it is likely that the secondary dressing will need to be removed and the primary dressing put back into its intended position.
Optimizing Healing Environment – Secondary dressings are often used to improve the healing environment beyond what the primary dressing provides. For example, absorbent dressings may help manage excess exudate. In this case, dressing wear time may be reduced if the medical adhesive used to secure the dressing is weakened by moisture from the exudate.
Holding Medical Devices in Place – Secondary dressings are also often used to help hold a catheter or other medical device in the wound area. It is important for the dressing to be very secure in these cases because it may be subject to excess pressure or pulling as the patient moves.
Incontinence – Secondary dressings can help protect the wound area from incontinence or other foreign substances. However, bodily fluids can also cause medical adhesives to lose strength, thus exposing the wound area to foreign debris and necessitating dressing changes.
The Role of Medical Adhesives
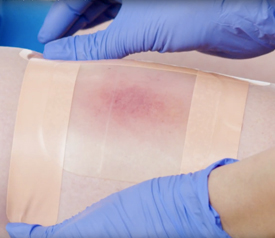
Medical adhesives play a major role in dressing security and wear time. In addition to remaining securely in place, dressings need to be easily removable to reduce periwound trauma or medical adhesive–related skin injury (MARSI). The most important step in improving wear time and skin protection is the application of skin protectant before dressing application. This is especially important for patients who are at higher risk for skin stripping or skin tears or who are sensitive to medical adhesives.
Dressings such as hydrocolloids may have integrated adhesive borders. However, this arrangement is usually not effective in many secondary dressing use cases. The dressing itself may range from mildly adhesive to non-adhesive. This is by design because the dressings should pull away easily and cleanly from wounded and healing or granulation tissue. Unfortunately, this means that without support, these dressings do not adhere securely to wounds.
To overcome this issue, some dressings come with an adhesive border. The hydrocolloid center covers the wound, and the adhesive is supposed to make contact with skin. In clinical practice, however, hydrocolloid dressings with adhesive borders are difficult to use, increase cost, and cause more waste. By using a gentle, strong, and waterproof medical adhesive, health care professionals can cut the dressing to the exact shape needed and be confident that the dressing will stay secure longer.
Conclusion
Secondary dressings can be an important part of the wound healing process. To be most effective, secondary dressings need to be securely held to the primary dressing. By using gentle, waterproof medical adhesives to secure secondary dressings, wound care clinicians can ensure exudate and other bodily fluids do not weaken the seal. This can lower the necessary frequency of dressing changes and help to lower costs.

