Preventing Skin Reactions to Glucose Monitors and Pumps
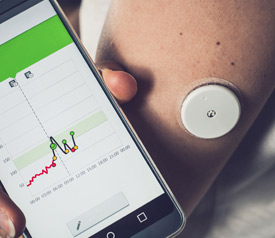
Continuous glucose monitors and insulin pumps have dramatically changed the way patients manage their diabetes. When these two devices are used together—one to sense blood glucose levels and the other to deliver insulin—they can perform like an artificial pancreas. Continuous glucose monitors and insulin pumps also promise far fewer fingersticks and insulin injections. However, as anyone who has a one of these devices will tell you, they can cause their own problems. One of the biggest problems with continuous glucose monitors and insulin pumps is what they do to the skin and underlying tissues. In this article, we provide some strategies for identifying and preventing skin reactions and ways to treat skin reactions to continuous glucose monitors and insulin pumps.
Common skin reactions to continuous glucose monitors and insulin pumps
Studies show that within 4 months of using an insulin pump, 9 out of 10 people will develop some sort of skin complication.1 About three-quarters of the time the devices cause at least moderate itchiness, two-thirds cause redness, and about half of the time they cause eczema.1,2 Perhaps more seriously, 1 out every 2 people who use insulin pumps develops some sort of skin wound, and scarring occurs in 94% of patients.1 In other words, these problems are common and potentially serious.
Continuous glucose monitors also cause a variety of skin reactions. Poor adhesion, skin irritation, and hypersensitivity (allergic reaction to the adhesives or other parts of the device) are quite common.3-6 A research group at Yale also found that sweating and activity leads to poor adhesion, which is related to skin irritation.6 People experience skin redness, chronically dry skin, and hyperpigmentation (a darkening of the skin). In one study, nearly 1 out of 5 people stopped using their continuous glucose monitor because of skin irritation or discomfort.7 While these devices can provide substantially better blood glucose control, that cannot provide these benefits if skin reactions make them unwearable.
Why does skin react to continuous glucose monitors and insulin pumps?
The skin and underlying tissues react to continuous glucose monitors and insulin pumps to cause irritation, discomfort and scarring in four major ways8:
- Hypersensitivity reactions – Skin exposure to chemicals in the devices and device adhesives over a long period trigger the immune system to develop an allergic reaction to these chemicals
- Contact dermatitis – Skin exposure to chemicals in the devices and device adhesives directly irritates the skin, causing relatively rapid inflammation and irritation (e.g., ethyl cyanoacrylates in a Dexcom G4 sensor adhesive9, isobornyl acrylate in the Freestyle Libre adhesive10)
- Scarring – This skin around the insertion site either becomes paler (hypopigmentation) or darker (hyperpigmentation)
- Lipodystrophy – The fat just below the skin either breaks down, leaving a depression, or grows abnormally, causing nodules under the skin.
Hypersensitivity reactions and contact dermatitis are mostly related to the adhesives that are used to hold continuous glucose monitors and insulin pumps in place. Scarring and lipodystrophy seem to be related to the infusion of insulin. Fortunately, scarring and lipodystrophy seem to be less problematic with newer insulin formulations and can be reduced by frequently rotating the devices to new areas.8,11 Therefore, we will focus our discussion on preventing hypersensitivity reactions and contact dermatitis to continuous glucose monitors and insulin pumps.
Preventing hypersensitivity reactions and contact dermatitis
It is difficult, if not impossible, completely void exposing the skin to the chemicals found in continuous glucose monitors and insulin pumps and their adhesives. Fortunately, manufacturers of these devices are working to make their adhesives less allergenic while providing stronger hold. Unfortunately, thousands of patients must struggle with hypersensitivity reactions and contact dermatitis until this is all sorted out. Fortunately, doctors and nurses who treat patients with these devices every day have come up with ways to approve adhesion and minimize risk. Their strategy is to properly prepare the skin and use high-quality medical tape to reinforce or replace the adhesives that are currently in these devices.
Tips for skin protection & Preventing Skin Reactions6,8,12
- Clean the skin with antimicrobial soap and dry the area completely
- Do not apply in a steamy bathroom; move to a place of low humidity and allow skin to cool after a bath or shower
- The area should be free of hair (a razor trim may be needed)
- If using alcohol to sterilize the area, try to keep it directly at the insertion site, not where the adhesive will need to stick
- If poor adhesion is a problem, apply a thin layer of antiperspirant to the area (make sure antiperspirant does not cause a skin reaction itself, though)
- If the skin irritation is being caused by the device itself (or device adhesive) use a tape barrier to prevent those areas from touching the skin; then use high-quality medical tape to hold the device in place; NOTE: For the most accurate results, the sensor should be placed on bare skin6
- Place the medical tape using a “picture frame” technique; use strips of medical tape to make a border around the device like the 4 sides of a picture frame or cut a hole in the middle of a patch of medical tape
- Use a waterproof medical tape that holds firmly but also releases gently and cleanly, without irritating the skin
- Remove tape using the “fold back” technique (slowly remove the adhesive at an angle, i.e., folding the tape back on itself)
Using Hy-Tape to secure in continuous glucose monitors and insulin pumps
Hy-Tape should be considered among the best tapes for securing continuous glucose monitors and insulin pumps. First, Hy-Tape is latex-free—latex is one of the most potent skin sensitizers found in medical products. No latex means no latex allergy. Hy-Tape also uses a zinc oxide adhesive that is gentle and even soothing on skin. It removes gently and cleanly, without leaving residue or damaging sensitive skin. At the same time, Hy-Tape is waterproof and adheres strongly enough to keep continuous glucose monitors and insulin pumps in place through sweating and activity. Lastly, Hy-Tape is thin and flexible; it can be used to secure continuous glucose monitors and insulin pumps in virtually any area on the body.
People who use continuous glucose monitors or insulin pumps to improve their blood sugar control are making a wise decision for their metabolic and overall health. Over time, most adjust to the day-to-day hassle of wearing these devices. Finding a way to secure these devices without irritating the skin may take a bit of trial and error, but following the tips listed above and choosing Hy-Tape for securement is a great place to start.
References – Preventing Skin Reactions
1. Berg AK, Olsen BS, Thyssen JP, et al. High frequencies of dermatological complications in children using insulin pumps or sensors. Pediatr Diabetes. 2018;19(4):733-740. 10.1111/pedi.12652
2. Binder E, Lange O, Edlinger M, et al. Frequency of dermatological side effects of continuous subcutaneous insulin infusion in children and adolescents with type 1 diabetes. Exp Clin Endocrinol Diabetes. 2015;123(4):260-264. 10.1055/s-0034-1394381
3. Englert K, Ruedy K, Coffey J, et al. Skin and adhesive issues with continuous glucose monitors: a sticky situation. J Diabetes Sci Technol. 2014;8(4):745-751. 10.1177/1932296814529893
4. Jadviscokova T, Fajkusova Z, Pallayova M, Luza J, Kuzmina G. Occurence of adverse events due to continuous glucose monitoring. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2007;151(2):263-266. 10.5507/bp.2007.044
5. Messer L, Ruedy K, Xing D, et al. Educating families on real time continuous glucose monitoring: the DirecNet navigator pilot study experience. Diabetes Educ. 2009;35(1):124-135. 10.1177/0145721708325157
6. Ives B, Sikes K, Urban A, Stephenson K, Tamborlane WV. Practical aspects of real-time continuous glucose monitors: the experience of the Yale Children’s Diabetes Program. Diabetes Educ. 2010;36(1):53-62. 10.1177/0145721709352010
7. Feig DS, Donovan LE, Corcoy R, et al. Continuous glucose monitoring in pregnant women with type 1 diabetes (CONCEPTT): a multicentre international randomised controlled trial. Lancet. 2017;390(10110):2347-2359. 10.1016/S0140-6736(17)32400-5
8. Messer LH, Berget C, Beatson C, Polsky S, Forlenza GP. Preserving Skin Integrity with Chronic Device Use in Diabetes. Diabetes Technol Ther. 2018;20(S2):S254-S264. 10.1089/dia.2018.0080
9. Schwensen JF, Friis UF, Zachariae C, Johansen JD. Sensitization to cyanoacrylates caused by prolonged exposure to a glucose sensor set in a diabetic child. Contact Dermatitis. 2016;74(2):124-125. 10.1111/cod.12503
10. Herman A, Aerts O, Baeck M, et al. Allergic contact dermatitis caused by isobornyl acrylate in Freestyle(R) Libre, a newly introduced glucose sensor. Contact Dermatitis. 2017;77(6):367-373. 10.1111/cod.12866
11. Richardson T, Kerr D. Skin-related complications of insulin therapy: epidemiology and emerging management strategies. Am J Clin Dermatol. 2003;4(10):661-667. 10.2165/00128071-200304100-00001
12. McNichol L, Lund C, Rosen T, Gray M. Medical adhesives and patient safety: state of the science: consensus statements for the assessment, prevention, and treatment of adhesive-related skin injuries. J Wound Ostomy Continence Nurs. 2013;40(4):365-380; quiz E361-362. 10.1097/WON.0b013e3182995516

